PROTECT | Values Guided Suicide Prevention
HEALING WITH HOPE | A Journey of Mental Wellbeing, Resilience, and Connection
Welcome to PROTECT, a transformative podcast dedicated to nurturing mental well-being, building resilience, and fostering hope. At its core, PROTECT is about the power of human connection—exploring how values like compassion, belonging, and loyalty can become lifelines for those facing challenges. Founded on the principle of Relational Safety, this podcast moves beyond traditional perspectives, asking not “what’s the matter with you?” but “what matters to you?”—empowering both professionals and individuals in their journey to chip away at pain and build strength.
Hosted by Dr. Manaan Kar Ray, an innovator and leader in mental health crisis care with over a decade of experience at Oxford and Cambridge, and now the Director of Mental Health Services at Princess Alexandra Hospital, Brisbane, PROTECT is changing the way we think about suicide prevention. Each episode blends leading-edge research with person-centered practice, bringing insights that promote hope, purpose, and resilience.
In our new focus, we introduce the STEPS 4 HOPE podcast series—an intimate exploration of suicide prevention through story, metaphor, and values-based connection. This season follows Ari’s Tapestry, a narrative journey through the six STEPS of suicidal distress: FABRIC, THREAD, NEEDLE, TIP, MEND, and FLOW. Each episode blends poetic storytelling, clinical insight, and emotional resonance to help listeners better understand what risk feels like—and how to respond with presence, curiosity, and care. Grounded in the HOPE framework, this series is a companion for anyone seeking to support others through pain, or to reweave their own path forward.
Whether you’re a clinician, caregiver, educator, or someone walking your own recovery journey, this podcast is an essential resource for all those who care deeply about mental health, suicide prevention, and building communities that thrive on connection and kindness.
Further information at www.PROGRESS.guide.
PROTECT | Values Guided Suicide Prevention
27 | Suicide Prevention for Health Regulators - Finding Common Ground
Use Left/Right to seek, Home/End to jump to start or end. Hold shift to jump forward or backward.
Would love to hear your thoughts...
A unique perspective to establish common ground between the Health Regulators and the practitioner under investigation is the basis for this episode. It builds on the previous episode of why Health Regulators need to be trained in Suicide Prevention and how Doctors and Nurses and Allied Health are an ultra high risk group when a notification happens.
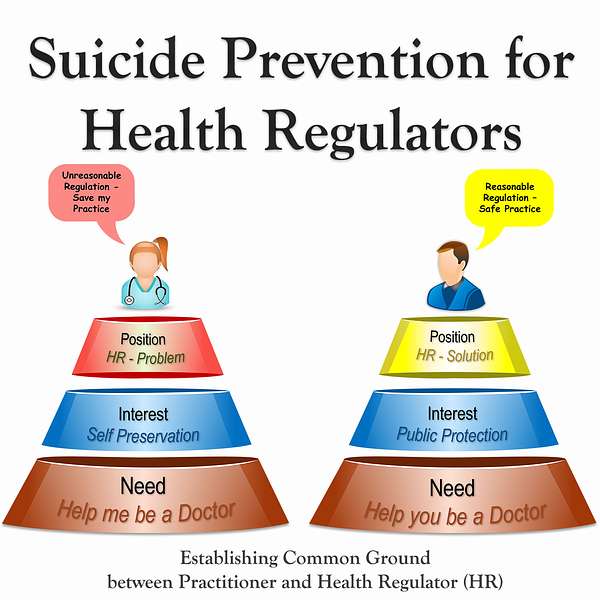
In this episode, Manaan shares how the practitioner considers the Health Regulator to be the problem where as the Health Regulators consider themselves to be the solution. These positions are incredibly divergent and the interests are different too, but at the needs level the doctors or the nurse wants to be a doctor or a nurse again and the health regulators role is to help them be one and practice safely in the long run. There is common ground to be found but the role of the health regulator in an investigation needs to be clearly articulated.
Connect with Assoc Prof Manaan Kar Ray on Linkedin
Follow us on www.progress.guide
Host: Good day and welcome to episode 27, I am Mahi your host and with me is Manaan, head of faculty for Progress Guide. As mentioned in the previous episode, we are going through an incredibly busy period of teaching, training, showcasing in the lead up to world suicide prevention day, so we are doing shorter podcast episodes. We do hope you too are getting ready in your organisation to observe world suicide prevention day. It gets the word out there, normalises talk about emotional pain and suicidal distress and fights stigma, we all have a part to play in suicide prevention.
Expert: I really do hope that mental health organisations in particular will utilise the day to spread the learnings from the different forums where deaths due to suicide get discussed like mortality and morbidity meetings, learning the lessons seminars, psychological autopsy case studies, reflective practice following serious incidents, you may call it differently in your organsiation based on where you are in the world but essentially the outcome is learnings, and the day can be used to thematically look at the key issues that have come up throughout the year in such meetings, and it will be a great opportunity to focus on 1, 2 or 3 improvement areas like enhanced safety planning, involvement of families in decision making, better safety documentation or seamless transition of care, improving 7 day follow up, whatever is the hot issue in your organisation, it is a great opportunity to focus in on that.
Host: I guess if you have willing member of a family who have been bereaved by suicide, they could share their story too and keep in sharp focus why this work is so important.
Expert: Data and numbers do tell a narrative, but there is nothing that moves health care practitioners than patient stories, brings to life the importance of the work they do. Fortunately for most mental health organisations in comparison to the number of people they serve, suicide is a rare event, devastating for those who have lost someone both family and the professional but it is rare. And days like this can also be used to build staff confidence and remind staff that it is a rare event, take time and pause and think, how many lives you have touched this year, we don’t tend to count non-events, and when a suicide does happen it is a reminder of the gravity of the work we do as mental health care professionals cause this could happen in any of those lives who are better of because you were present in their moment of extreme distress, you brought comfort and you brought hope. So it is important to remember that too.
Host: That is so true, so you can learn a lot more from what worked well and then look at even better if…
Expert: The whole ethos of appreciative enquiry and curiosity is quite an inspiring approach to continuous improvement. It is embedded in Restorative Just Culture, we might do a few episodes along the line on Just Culture.
Host: So today you wanted to do a wrap up of the Suicide Prevention Training for Health Regulators.
Expert: Yes, on the 11th of August we delivered the adapted version of PEARLS for the clinical input team at AHPRA.
Host: How did it go?
Expert: Yes, very well, really engaged audience, very keen to learn.
Host: What was the composition of the attendees?
Expert: All sorts but most of them were from a legal background, some from the police as well, and in the interactive evaluation we did 35% rated themselves as novices in the field of suicide prevention, which is not surprising. 15% considered themselves proficient and I am assuming they are the ones from a health or mental health background.
Host: And how frequently do they encounter suicidal distress in health practitioners?
Expert: About 85% were distributed between the once in a quarter and the half yearly rating and 15% were in the weekly, fortnightly and monthly categories. I don’t know how the case distribution happens, and whether particular types of health professionals with mental health related issues are allocated to those with a mental health background or not but I was left wondering that if that isn’t the case, then why is there such a big disparity between the same cohort of people doing the same kind of work.
Host: Will you get to find out about how the case allocation happens?
Expert: Yes, I will have a debrief with Tamzin Mondy the National Manager for the Clinical Input Service, and I do intend to find out. If there is not a particular way of prioritising the case allocation, then we are in that territory of the eyes can’t see what the mind doesn’t know, or in this the ears cant hear what the mind doesn’t know. It may very well be that those who have a mental health background are able to see things and hear things that those with a legal background are not able to, and it will be unfair to expect a legal practitioner to pick up subtle signs and symptoms in conversation in the same way a clinical psychologist will.
Host: Yes, that will be like comparing apples and oranges.
Expert: Yes, and that in itself makes the case for training and upskilling of people who have not got the background, as we explained in the previous podcast doctors and nurses because of there professional background, knowledge of the human body, access to means and desensitisation to pain and death can do some serious harm to themselves when they develop a strong desire to escape the emotional pain that a notification might cause.
Host: Yes, and you talked about joiner’s model of perceived burdensomeness, failed belongingness and acquired capability.
Expert: And to that you can add the volitional factors from Rory O’ Connor’s Integrated Motivational Volitional model or the practical capacity to progression from ideation to action from Klonsky’s 3 step theory, essentially I am repeating the whole issue of access to means and knowledge of human physiology to go with the acquired capability. Actually Kolnsky’s second step is also quite relevant, he talks about pain exceeding connectedness on step 2 when there is an escalation from ideation to intention formation, so modest or passive ideation becomes strong / active when pain precludes the experience of connectedness to loved ones, valued roles and sense of meaning and purpose, it is similar to Joiner’s perceived burdensomeness and failed belongingness in that sense. But what is striking is how most contemporary models put health professionals in that ultra high risk group who have the make up to take catastrophic steps to break out of the entrapment of life.
Host: Did you go into details of these models?
Expert: No not really, as I said the group was very diverse and you know how we do the digital interactive precourse survey about one thing that you hope to learn today, one skill that you hope to gain today, we use that to flex any course to the needs of the audience. And a lot of the answers were about how to support a person in the moment, the most respectful way to communicate, to show genuine empathy, identifying red flags, a lot do with conversations and communication, there were some interesting request about managing self in the moment, supporting colleagues as well and also about creating hope for the health practitioners.
Host: So, there was this understanding in the room as to why a health practitioner may be feeling hopeless when they are undergoing an investigation.
Expert: Oh yes, they came across as a very switched on bunch. I think the issue is that a lot of them are from a legal background where things are right or wrong, black or white, shades of grey and ash are quite difficult to conceptualise and mental health is all shades of grey and ash.
Host: In the courses you run often we get to see those ah ha moments, were there any such moments.
Expert: Yes, I think so, saying that it is much more difficult to pick them up when online particularly if a large bunch is sitting in one room so you haven’t got the camera just on their face. There was one specific moment, which really did stand out for me which was around the purpose of those in the clinical input team, why they get out of bed in the morning.
Host: Can you share more.
Expert: You know how if you are case managing an investigation, you are perceived by the health professional in an adversarial role, but if the notification is for a health reason, yes the regulator has to ensure that the practice of the practitioner is safe, but surely the overall aim of the health regulator is to support the practitioner to get back into practice, safe practice but get them back practicing again. So as I tend to do, I digress and go off message and I started talking about the why? What is your why? Why do you get out of bed every morning? Surely there can be no greater motivation than reconnecting a doctor, a nurse or an allied health professional back with patients. Cause through that health professional you are influencing and touching the lives of hundreds of thousands of people.
Host: Hundreds of thousands?
Expert: Yea do the maths. Lets pick an ED physician, in a year they will see perhaps 5,000 patients, if they have 30 years left in there carrier , that is straight away 150,000 patient that this doctor will see and support and they wouldn’t have done so if they were not ably supported to get back into practice safely, and who does that it is the clinical input team, that’s there role to make sure that the practice is safe and sustainable and they stay well and keep practicing. Every year that ED Consultant will train up two registrars as a bare minimum, 6 months each, so in the next 30 years that’s 60 registrars, and then each of those registrars will see 150,000 to 200,000 patients each in their life time, multiply that figure by 60, you start getting into some seriously big numbers.
Host: Yes 60 times 200,000 is 12 million people.
Expert: See, each doctor, each nurse has huge impact on the community they serve. And if they cannot work because of a health reason, that is a huge loss to society, and that is where the clinical input team can make a massive difference to the life of the health practitioner, their family, their projected future, they patients they will support, the juniors they will train, the community they will support. So these people that I interacted with in AHPRA are at the cross roads of someone’s carrier, they can make it or break it, surely the goal is to reunite them with life’s purpose, i.e. treating patients, supporting people, their passion, their purpose, what brings meaning to their life. This is what the health practitioner has worked for their entire life and those working in the clinical input unit can help get their life back on track again.
Host: When you think about what motivates staff in the clinical input unit, I can see when you frame it in the way you have done why it will feel more motivating, this is a much better narrative where you are enabling doctors and nurses rather than waking up and going to work to stop health practitioners from practicing. But did the message get through.
Expert: I think so, from the expressions I saw on people’s face, it felt like an ah ha moment.
Host: But this is a different lens to look at one’s role within AHPRA, how do you get past that adversarial perception that the health practitioner has.
Expert: For starters, kindness and compassion in the words we pick goes a long way in diffusing that tension in the role, that is the how, how we interact, howe w converse with the health practitioners, however I feel that this goal, this why we have been talking about, why we do what we do needs to be clearly articulated to the health professionals. We are both working towards the same goal, which to get you back practicing, ensure that your practice is safe, ensure that you stay well and your health and practice is sustained in the long term future.
Host: So actually explain their role in the process of the notification and investigation?
Expert: Yes, why not. One can use the model that we use for the pain relief conversation. I think episode 5, so listeners can go back to that episode to have a listen as to you help a person in suicidal distress see overlapping goals. So a brief recap, we had the person in suicidal distress and the professional on different hills and on each hill we had a top tier of position, below it interests and below it needs. The person has taken up the position of dying and considers suicide to be the solution, and the professional has the position of living and views suicide as the problem. We recommend that the professional digs deep to establish the interests and needs that underlie the position of dying. When faced with the ambivalence a person is experiencing towards life, it is strongly recommended to avoid a power struggle. Professionals need to temporarily relinquish their strong desire to pull over the person from their death orientation to one of living. This requires courage as it might go against all that the professional believes in and is trained in. Gain an understanding of how the underlying interest to escape entrapment and the need to be pain-free manifests as suicidality. Construct a pain based narrative and help the person see that their desire to eliminate excruciating pain is a justifiable response, a response they share with all other living beings. This validation will goes a long way in establishing the safety partnership. Seek first to understand and then to be understood. Once you have been able to help them see that there need is pain relief, you can then begin to say that your role is to explain alternatives and help them be pain free, together you all can do things to chip away at the pain or improve your tolerance to the pain. Essentially what you have done is you have avoided a power struggle and helped the person in distress see that there is common ground with overlapping needs so there is every reason to work together.
Host: Yes, I remember that, I think episode 5 is one of the most listened to episode as well, this model is so elegant and simple to comprehend, how does this apply to the APHRA situation though.
Expert: Well here too you have two hills, you have the health practitioner who has been notified on one hill and you have the case manager from AHPRA on the other hill. The health practitioner see AHPRA as the root of all their problems, in fact they view AHPRA and the case manager as the perpetrator or enforcer of expectations that they often consider unreasonable.
Host: So are you saying that the AHPRA case manager thinks that AHPRA’s position is reasonable or AHPRA’s actions are reasonable and the health practitioner’s position is AHPRA’s actions are unreasonable.
Expert: Yes, so the health practitioner thinks, AHPRA is the problem, the case manager from AHPRA thinks AHPRA is the solution. When you begin to dig deep and look at what are the interests that underlie the position, the health practitioner’s interest are to do with self preservation, all that they have worked for in their life is under risk or under scrutiny is being investigated, so understandably the amygdala kicks in, so self preservation as the interest on one hill and the other hill the primary interest is public protection through practice regulation, ensuring standards are upheld.
Host: So that still feels quite adversarial
Expert: Yes, it does, but if you go a layer deeper, you find that at the level of needs the health professional is saying, help me be a doctor (again), help me be a nurse (again), or whichever professional background they belong to, that is there need. Now for AHPRA the need is not that different, as I was explaining before, there ultimate need is to ensure that doctors and nurses are out there practicing, yes as a regulator they want to make practice safe, but surely that is something that the doctor or the nurse wants to, cause for them to be a doctor or a nurse in the long run there practice has to be safe. Effectively, if the AHPRA case managers can explicitly talk about their role, they can share with the health practitioner and their defence union or supporting people, hey you want to be back practicing again and my role is to help you be back practicing again, and the way I am going to help you achieve what you want achieve is by ensuring that your practice is safe. You need is to be a doctor again and my need is to help you be a doctor again.
Host: So, there is common ground.
Expert: Absolutely there is, but a concerted effort has to be made for the health regulators to help the health practitioner see that cause at the level of positions, it feels extremely adversarial.
Host: This is a very different lens for the case managers to view the work they do, overall though how did the pre and post-course ratings go?
Expert: Very well actually this was a PEARLS masterclass, which is normally 2 hours but we did an extended one with them for 3 hours, and 3 hours is not long at all, and in that short window the pre course rating of feeling confident in supporting people in suicidal distress shifted from 5.6 on a 10 point scale to 7.6, that is quite a significant improvement in a short window.
Host: That is, given a lot of people were from a legal background as well.
Expert: And what was most pleasing to see was that the highest improvements were in their ability to connect with empathy, their understanding of the origin of suicidality as well as in their confidence to ask about suicidal thoughts and feelings. After the morning masterclass in the afternoon they had a session thinking through how they will put into practice the knowledge they have gained, and when I have my debrief with Tamzin I will get to know more about it. Had some lovely email feedback as well from attendees as to how useful they found it and that is always pleasing. I do feel that the balancing act regulators have to do is incredibly difficult.
Host: Yes you picked up a bit of flack on Whatsapp, didn’t you?
Expert: Good lord yes, so I tend to post the podcast on a number of whatsapp groups that I belong to, mainly made up of doctors and some of the views people expressed was quite stark. Its there opinion and they are allowed to have one and although I was tempted to respond I didn’t, but I did feel that many do not appreciate how difficult the balancing act is for AHPRA in between public protection and ensuring that the health practitioner can get back to doing what they have worked there entire life towards doing. Most were appreciative of the work that I am doing with AHPRA but they hold some strong views.
Host: And those views take a long time to shift.
Expert: Yes, and actions speak louder than words and it is a long road for AHPRA to prove through there actions that they can be kind and compassionate regulators and through the process of regulation produce better doctors and nurses and allied health professionals. I think that is Martin’s end game for Aphra, but a journey of a thousand miles
Host: Begins with a single step, I thought we were going to do shorter episodes while we went through the busy period in August and September.
Expert: Well, we begin chatting and time flies when you are having fun.
Host: So, you are going to be doing Hong Kong this week.
Expert: Actually, by the time the episode airs on Friday, I would have completed the bulk of the big bang PROTECT training.
Host: So, what are you delivering.
Expert: On the 16th and 17th of August I will train the School Counsellors and Educational Psychologists from 22 schools in the English Schools Foundation on PROTECT, 6 of them will become protect guides as part of our training the trainer offering. On the 18th of August we will be training up teachers across the 22 schools in LIFE, about 25 of them will become LIFE guides, who can then deliver LIFE to other teachers as well as PEARLS to students. And then finally on the 22nd Monday we will be back to the School Counsellors again, to run the 7 SAFE Steps program, where they practice the skills.
Host: You love that program don’t you.
Expert: Yes, I think it is the professional actors that we have, they are so good in making it real and keeping it grounded.
Host: Which case study are you doing?
Expert: It’s a new case study actually, not Sandeep or Sandeepa, its Sam, but more about that next week.
Host: Cant wait to hear about the new case study. And you are training GPs on the 30th August.
Expert: Yes, that is in the UK with Sutton Coalfields Clinical Commissioning Group. Love training up GPs as they see so many people in suicidal distress, it is a daily affair and they have so little time to train, but it is essential that they have the skills to support people in suicidal distress particularly those with chronic suicidality, as often they have short periods of support in secondary care but the bulk of the support is in primary care.
Host: You wanted to talk about the whole of school approach to suicide prevention today but we have run out of time.
Expert: Yes, we can pick that up in the next episode, really excited to be part of this partnership with ESF in Hong Kong, some of the emerging covid data for 2021 shows that the impact on young people has been immense.
Host: Seems like we will be staying with COVID for a very long time, both in terms of the recurring waves that come as well as the longer term psychological impact.
Expert: Indeed, but I would like to believe that the worst is behind us.
Host: Certainly, hope so. We have come to the end of today’s episode, today you learnt about an innovative application of the pain relief conversation, how one can use the positions, interests and needs model in a completely different context to find common ground. Hopefully health professionals listening to this podcast will have a better understanding of the regulators role and if those who attended the PEARLS course on the 11th August hear this, for them it will refresh there why, there purpose and the impact they have on larger society and the community by helping health practitioners who have have had a health notification return back into practice. In the next episode we will delve into suicide prevention in schools and universities. Today’s episode has come close to normal length although our intention was to do shorter episodes. There are other talks from Manaan in the lead up to the world suicide prevention day, on the 31st of August for Lifeline Western Australia, that’s at 7:30 pm Australian Eastern Standard Time, i.e. Brisbane Time. It is an overview talk PROTECT LIFE PEARLS: Practical Suicide Prevention Skills from Hospital to Schools and then there is the UK suicide prevention summit hosted by Mental Health Academy on World Suicide Prevention Day itself on Critical Crisis Care Conversations in Borderline Personality Disorder. That’s on the 10th of September, Brisbane time 8 pm. Hope you are making plans in your organisation too as to how to observe world suicide prevention day on the 10th of September, every 40 seconds a life is lost to suicide and awareness about what we can individually do can save a life, a life who is someone’s father, mother, brother, sister, son, daughter, husband, wife, friend, you can play a part in the fight against suicide, I hope you do, catch up next Friday, in the interim make time to ask someone, R u ok and if they are not make time and space for them and convey that it is ok to not be ok and they in time will pay it forward.

