PROTECT | Values Guided Suicide Prevention
HEALING WITH HOPE | A Journey of Mental Wellbeing, Resilience, and Connection
Welcome to PROTECT, a transformative podcast dedicated to nurturing mental well-being, building resilience, and fostering hope. At its core, PROTECT is about the power of human connection—exploring how values like compassion, belonging, and loyalty can become lifelines for those facing challenges. Founded on the principle of Relational Safety, this podcast moves beyond traditional perspectives, asking not “what’s the matter with you?” but “what matters to you?”—empowering both professionals and individuals in their journey to chip away at pain and build strength.
Hosted by Dr. Manaan Kar Ray, an innovator and leader in mental health crisis care with over a decade of experience at Oxford and Cambridge, and now the Director of Mental Health Services at Princess Alexandra Hospital, Brisbane, PROTECT is changing the way we think about suicide prevention. Each episode blends leading-edge research with person-centered practice, bringing insights that promote hope, purpose, and resilience.
In our new focus, we introduce the STEPS 4 HOPE podcast series—an intimate exploration of suicide prevention through story, metaphor, and values-based connection. This season follows Ari’s Tapestry, a narrative journey through the six STEPS of suicidal distress: FABRIC, THREAD, NEEDLE, TIP, MEND, and FLOW. Each episode blends poetic storytelling, clinical insight, and emotional resonance to help listeners better understand what risk feels like—and how to respond with presence, curiosity, and care. Grounded in the HOPE framework, this series is a companion for anyone seeking to support others through pain, or to reweave their own path forward.
Whether you’re a clinician, caregiver, educator, or someone walking your own recovery journey, this podcast is an essential resource for all those who care deeply about mental health, suicide prevention, and building communities that thrive on connection and kindness.
Further information at www.PROGRESS.guide.
PROTECT | Values Guided Suicide Prevention
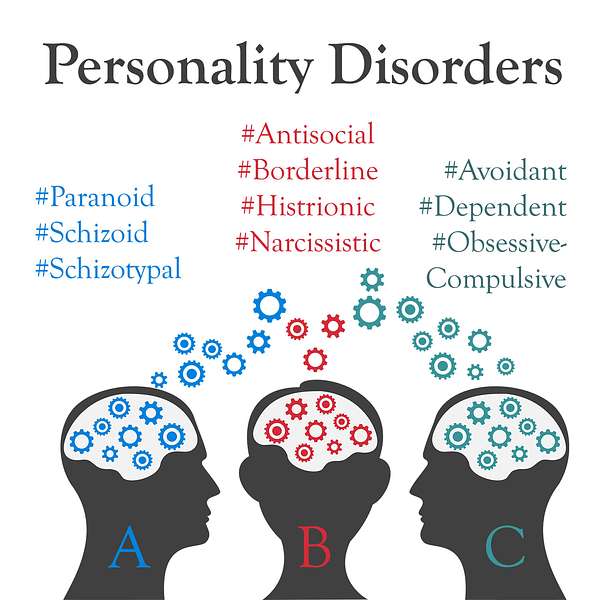
20 | Personality Disorder ~ Clusters A, B and C
Use Left/Right to seek, Home/End to jump to start or end. Hold shift to jump forward or backward.
Would love to hear your thoughts...
In the lead up to a case study, Manaan delves deep into Personality Disorders and talks about all 10 conditions covering clusters A, B and C in this episode.
Cluster A
These personality disorders are characterized by odd or eccentric behaviour. People with cluster A personality disorders tend to experience major disruptions in relationships because their behaviour may be perceived as peculiar, suspicious, or detached.
Cluster B
The cluster B personality disorders are characterized by dramatic or erratic behaviour. People who have a personality disorder from this cluster tend to either experience very intense emotions or engage in extremely impulsive, theatrical, promiscuous, or law-breaking behaviours.
Cluster C
Cluster C personality disorders are characterized by anxiety. People with personality disorders in this cluster tend to experience pervasive anxiety and/or fearfulness.
Connect with Assoc Prof Manaan Kar Ray on Linkedin
Follow us on www.progress.guide
Host: Good day, this is Mahi, your host, we are on to episode 20, we began the ASSESS module in Episode 13, Manaan provided an overview and we started looking at attitudes to suicide and why awareness regarding where one stands is so important in terms of care delivery. In Episode 14 we went deeper into the first chapter of ASSESS, appraise decisions and began the AWARE framework. Manaan, given we will do a case based discussion do you want to provide a summary of AWARE.
Expert: Sure, so in Episode 14 we discussed the impact of anxiety on decision making and how assessments have a dual role, the overt stated one i.e. to assess and the subtle implied one i.e. to contain the crisis and how these two functions can be at cross purposes and how anxiety of unearthing things that are difficult to contain may get in the way of a full through exploration. In episode 15 we built on this concept further and discussed two mental spaces, rational and rationalizing. So rational is information first, decision later and rationalizing is decision first followed by selection of information to support the decision or action. We then explored W for weighting in episode 16. How much weighting assessors put on certain diagnostic groups namely personality disorder, and substance misuse and how suicidality in these groups often count for less, also how an acute course of illness gets more priority than chronic although those who are chronically unwell may have lost touch with hope and finally how suicidality caused by modifiable social factors are often considered by healthcare staff as outside their core remit of work and these patients end up receiving less support than those with a clear cut biological mental illness. In episode 17 we explored two AWARE factors. A for Agenda and R for Resources. We talked about how an assessment get skewed by the agenda that the assessor perceives, this may be in the referrer, patient or family. We then explored resources, whether that be beds or workload in a team and its impact on decision making. We again talked about the two mental spaces, rational and rationalizing, how tempting it is to justify a resource led decision as one that has been taken in the patient’s best interest. Staying in the rational space does not suddenly give us more beds, but we are more aware of the risks involves as we have not rationalized them away thus we might engage in far more stringent safety planning. In episode 18 we had a detailed discussion about the final AWARE factor, E for Experience. We discussed how past experience influences clinical decisions, whether that be the experience of supporting the same patient previously or a different patient from the same diagnostic or demographic group. We also talked at length about the professional or personal experience of suicide, ways in which it may help and ways in which it may impede.
Host: In episode 19 you built on this discussion about experience further and introduced the phenomenon of Creep – Crash – Crawl .
Expert: Understanding Creep – Crash – Crawl is essential to ground risk thresholds. It describes how risk taking while supporting those in suicidal distress goes up over time due to suicide fortunately being a rare event. Every time a clinical decision is made that does not result in harm to the patient, the assessor believes that it was ok to take the risk, it was ok not because it was a clinically sound risk, it was ok because as an outcome, suicide is rare. So the risk taking threshold gradually creeps up to the point that it is unsafe and then there is an unfortunate event. At the face of it the person who suicides, there is not much that differentiates them from the 10-20-30 others that the clinician might have assessed that month or that year, when risk gradually rose up. Once a suicide happens it does impact the confidence of the clinician and then positive risk taking crashes through the floor and crawls along for a while as the clinician goes through the process of soul searching and the organization scrutinizes the incident with the benefit of hind sight. This crawl phase results in restrictive practice which is quite detrimental to the person being supported as it destroys agency and self belief in the person, essentially the confidence of the assessor gets mirrored in the person.
Host: With this context in mind let’s provide you with the first of our case studies. But first the disclaimer - all the case studies, i.e. characters and events discussed in all our podcasts are fictitious. Any resemblance to a person living or dead is purely coincidental.
Expert: Actually this is a fairly important point. When health professionals communicate with each other they use diagnostic groups. For example when a GP would write a letter to me referring a person they may say that Mr Smith suffers from depression, we would like your opinion on his pharmacological management. Given GPs spend about 10 minutes with a patient they cannot realistically spend more than a minute to write a letter or else it begins to impact on the care that they will provide. So the word depression becomes the proxy for a range of symptoms, low mood, tearfulness, lack of pleasure, lack of energy, poor concentration, low self esteem, low self confidence, worthlessness, helplessness, hopelessness, suicidal thoughts, plans, actions and a range of vegetative symptoms relating to appetite, weight, sleep and sex drive. Now every patient has not got all the symptoms of depression, they will have some of them and their source of pain will be unique, but there will be more similarities than dissimilarities within a diagnostic group, so the word depression becomes a way in which one can save time. People may criticize this reductionist approach towards human beings and that human beings are people and not diagnosis, but in terms of communication that is the purpose to save time. There are a whole host of other reasons which relate to the foundations of evidence based care but lets not go into that. The reason I am elaborating the disclaimer is because when we go through a case study we will state symptoms of a particular diagnostic group, and if people living with mental health challenges listen to the podcast, it will appear that as if we are talking about you. Particularly people that I have cared for personally as a Psychiatrist may feel that I am publicly saying things that relate to them. But please be assured that is not the case. All case studies are fictitious, we use the diagnostic criterion to construct their symptoms and give their stories events that normally people living with that diagnosis repeatedly present with, so all resemblances are fictitious.
Host: Now that we have got that out of the way, lets get into the case study. I understand you wanted to explore how the AWARE factors relate to people living with a diagnosis of Borderline Personality Disorder.
Expert: Yes, that’s correct.
Host: Do you want to take us through what is a personality disorder first and then what is a borderline personality disorder, before we get into the case study.
I think that is a good idea, as there is a lot of stigma attached to the word personality disorder and the light of knowledge is the best way to combat the darkness of stigma. We may not get around to the case study in this episode, if we delve deep into personality disorders, but so be it, I think that is time well spent.
Host: And that is because there are 10 different Personality Disorders?
Expert: Yes, that is right, there are 3 clusters, A, B and C. Clusters A and C have 3 diagnostic groups each and cluster B has four.
Host: I have a feeling this is going to get very clinical
Expert: Well, it does not need to be. I will try and keep things simple. Our personality is the collection of thoughts, feelings and behaviours that makes each of us the individuals we are. We don't always think, feel and behave in exactly the same way – it depends on the situation we are in, the people with us and many other interconnecting factors. However, if you experience significant difficulties in how you relate to yourself and others and have problems coping day to day, you may receive a diagnosis of personality disorder. So personality disorders in general are pervasive across time and settings, and one can see enduring patterns of thinking, perceiving, reacting, and relating that cause significant distress or functional impairment in other words it affects a number of aspects of life.
Host: So they are like personality traits.
Expert: Traits too represent patterns of thinking, perceiving, reacting, and relating that are relatively stable over time. However, for those living with personality disorders, their traits become so pronounced, rigid, and maladaptive that they impair work and/or interpersonal functioning. It is important to remember that people with personality disorder are not broken, they think differently and experience the world in a different way... and given we all have unique life experiences that impact the way in which we respond to the world around us, and no one really is in anyone else’s shoes, there should be no judgement and there's no shame in doing whatever someone needs to do to cope with their emotions in a safe and supportive way
Host: Is it just life experiences that cause Personality disorder?
Expert: Well, each conditions varies significantly in their manifestations, but all are believed to be caused by a combination of genetic and environmental factors. Whatever be the cause It is important to remember that we all have parts of our personality that can cause us or others difficulties. What is different for people with personality disorders is the intensity of these difficulties and the fact that they might need extra support. Many gradually become less severe with age, but certain traits may persist to some degree after the acute symptoms that prompted the diagnosis of a disorder abate. Diagnosis is clinical. Treatment is mainly with psychosocial therapies and sometimes drug therapy.
Host: So what are the different Clusters and the different conditions.
Expert: As mentioned currently psychiatrists tend to use a system of diagnosis which identifies ten types of personality disorder that are grouped into three categories or clusters. Cluster A is characterized by high levels of suspicion and people may not conform to social expectations, appearing odd or eccentric or suspicious. The 3 in this cluster are Paranoid personality disorder, Schizoid personality disorder and Schizotypal personality disorder.
Host: Lets begin with Paranoid personality disorder
Expert: This is characterized heavily by mistrust and suspicion. This means that they find it hard to confide in people, even their friends and family, they find it very difficult to trust other people, believing they will use them or take advantage of them, they have difficulty relaxing and read threats and danger (which others don't see) into everyday situations, and even innocent remarks or casual looks from others may bring out an extreme response.
Host: The next two, Schizoid personality disorder and Schizotypal personality disorder, they sound like Schizophrenia, are they the same.
Expert: For Schizoid personality disorder the primary characterization is one of disinterest in others, many are able to function fairly well. Unlike in schizophrenia or schizoaffective disorder, they would not usually have psychotic symptoms. However, as a result of the thoughts and feelings associated with this diagnosis they may find difficulty forming close relationships with other people, choose to live their life without interference from others, prefer to be alone with their own thoughts, pleasure in activities is limited and they have little interest in sex or intimacy, they may come across as cold towards others.
Host: What about Schizotypal, is that similar to Schizophrenia.
Expert: I guess being eccentric is the defining characteristic of Schizotypal personality disorder but everyone has their own eccentricities or awkward behaviours. But, unlike schizophrenia, they would not usually experience psychosis, their patterns of thinking and behaving make relating to others very difficult. They may experience distorted thoughts or perceptions, find making close relationships extremely difficult, think and express themselves in ways that others find 'odd', believe that they can read minds or that they have special powers such as a 'sixth sense', feel anxious and tense with others who do not share these beliefs and feel very anxious and paranoid in social situations.
Host: So those are the 3 in Cluster A, what defines Cluster B?
Expert: People living with a Cluster B diagnosis may come across to others as dramatic, emotional, or erratic. There are four in this group: Antisocial personality disorder (ASPD), Borderline personality disorder (BPD), Histrionic personality disorder and Narcissistic personality disorder.
Host: Antisocial, does that include 'psychopathy' and 'sociopathy'?
Expert: Yes, it does, it is natural to sometimes put our own needs, pleasure or personal gain before those of others around us. However, if these actions occur very frequently and one struggles to keep stability in their life, or they regularly act impulsively out of anger or lack of consideration for others, this could lead to a diagnosis of antisocial personality disorder. So those with this diagnosis often act without thinking about the consequences for themselves or other people and put themselves in dangerous or risky situations, behaving sometimes illegally and their behaviour may be unpleasant for others. They may be aggressive, in frequent fights, and struggle with having empathy for others and hurt others without showing guilt or remorse.
Host: So putting it bluntly social irresponsibility, disregard for others, deceitfulness, and manipulation of others for personal gain. I have read about people with ASPD having criminal records and when they were young they may have had conduct problems.
Expert: Yes, that is correct, most would have had a diagnosis of conduct disorder in their younger years
Host: The next one is Borderline Personality Disorder
Expert: Now that is characterized by Inner emptiness, unstable relationships, and emotional dysregulation, but I might save it for the next episode as our case study Jill will have a borderline personality disorder and that way it will be fresh in our listeners minds. I don’t think after going through all 10 conditions today we will have time to discuss the case study as well.
Host: Fair enough, so moving on, the next is Histrionic personality disorder.
Expert: This is characterized in pejorative terms like being attention seeking.
Host: Almost the dictionary meaning.
Expert: Well, there is also excessive emotionality. Most people enjoy being given compliments or positive feedback about their actions. But if they depend very heavily on being noticed, or are seeking approval so much that this affects their day-to-day living, they might get this diagnosis. So if they are not the centre of attention they may feel very uncomfortable, almost a compulsion to entertain others and constantly seek, or feel dependent on, the approval of others, the desire to stay as the centre of attention may result in flirting or dressing provocatively or making rash decisions, unfortunately all of this may result in a reputation of being dramatic.
Host: And finally in Cluster B, Narcissistic, is that to do with self-grandiosity.
Expert: And also need for admiration, and lack of empathy. It is human nature to be aware of our own needs, to express them, and to want others to be aware of our abilities and achievements. Self promotion is a reality of modern western living. One could even class it as not a bad trait. However, if these thoughts, feelings and behaviours are very extreme and cause problems in relating to others, one should consider a diagnosis of narcissistic personality disorder.
Host: So if you are living with a person with Narcissistic personality disorder, what do you actually get to witness.
Expert: They believe that there are special reasons that make them different, better or more deserving than others, they have fragile self-esteem, so that they rely on others to recognise their worth and their needs. They feel upset if others ignore them and don't give them what they feel they deserve, and resent other people's successes, put their own needs above other people's, and demand others put them ahead too. So they may be seen as selfish and dismissive or unaware of other people's needs.
Host: This brings us to Cluster C. I understand it is characterized by appearing anxious or fearful.
Expert: Yes, that is correct, the 3 in this group are Avoidant personality disorder, Dependent personality disorder and Obsessive compulsive personality disorder.
Host: So, I am assuming Avoidant will involve avoidance of relationships like interpersonal contact.
Expert: Yes, due to high levels of sensitivity to rejection.
Host: But we all have things, places or people we don't like, which make us anxious.
Expert: But if these things cause so much anxiety that one struggles to maintain relationships in their life then it’s a problem.
Host: So, does it primarily feature with worries about being rejected and ridiculed
Expert: It can, well people avoid work or social activities which needs them to be with others, they are forever expecting disapproval and criticism and become very sensitive to it. They worry constantly about being 'found out' and rejected or being ridiculed or shamed by others. They avoid relationships, friendships and intimacy because they fear rejection, so they feel lonely and isolated, and inferior to others. They are reluctant to try new activities in case they embarrass themselves.
Host: How does Dependent personality disorder differ from Avoidant
Expert: Well, they are in the same cluster because of their similarities. The main characteristic in Dependent personality disorder is one of submissiveness and a need to be taken care of.
Host: But it is natural to need other people to care for us or give us reassurance sometimes.
Expert: Yes, but a healthy balance involves being able to both depend on others as well as being independent from others sometimes. However, if feelings and thoughts about needing others become so overwhelming that they impact your daily life and relationships, then a diagnosis of dependent personality disorder should be considered.
Host: So do people come across as needy and 'weak'
Expert: Yes they do, they are unable to make decisions or function day-to-day without help or support from others, they allow or require others to assume responsibility for many areas of their life, they agree to things they feel are wrong, they avoid being alone or losing someone's support and are very afraid of being left to fend for themselves due to low self-confidence, seeing others as more capable than themselves.
Host: The last of the 10 Obsessive-compulsive personality disorder, is that similar to OCD?
Expert: Put bluntly perfectionism, rigidity, and obstinacy are the key characteristics. OCD or obsessive compulsive disorder is separate to obsessive compulsive personality disorder, OCD is not as such is not based on a type of personality, it is a behaviour based disorder although there is overlap like problems with perfectionism, the need for control, and significant difficulty being flexible in how someone thinks about things.
Host: So, they need to keep everything in order and under control.
Expert: Yes, the pillows on the bed, the books on the shelves and the jackets in the wardrobe. They also set unrealistically high standards for themselves and others, with their own way being the best. They want things just so i.e. get worried if they are not perfect and they also worry about others making mistakes.
Host: That is a lot of information about personality disorder, will you provide a summary.
Expert: Ok so 3 clusters, 10 disorders, Cluster A includes personality disorders that are characterized by odd or eccentric behavior. They tend to experience major disruptions in relationships because their behavior may be perceived as peculiar, suspicious, or detached. Cluster B personality disorders are characterized by dramatic or erratic behavior. They tend to either experience very intense emotions or engage in extremely impulsive, theatrical, promiscuous, or law-breaking behaviors. The most common clinical presentation is Borderline Personality Disorder, that’s what its called in DSM5, In ICD the same condition is called emotionally unstable personality disorder, perhaps a more descriptive and less stigmatizing name. and finally Cluster C personality disorders are characterized by pervasive anxiety and/or fearfulness.
Host: That is an excellent summary, we never got around to Jill our case study as we ran out of time, but we promise to talk about Jill next time and how the AWARE factors relate to Jill. We will also spend time delving deeper into Emotionally Unstable Personality Disorder or Borderline Personality Disorder. Today’s episode was a very content heavy episode based on factual knowledge. Pause and think about your clinical practice and what challenges you face with specific personality disorders. If you have specific questions please do email us at admin@progress.guide. Share your musings with us. Tweet your thoughts about weighting and tag #GuideProgress. It helps get the word out about the podcast to more professionals and support progress to practice. You can access all the transcripts at www.progress.guide. You can connect with Manaan on Linked in, or follow our linked in page by searching on linked in for progress.guide. We are also on twitter and YouTube. Our twitter handle is @GuideProgress. As usual please do follow the podcast, there will be weekly episodes every Friday and share it with your colleagues. Your ratings will help get the word out so please don’t forget to rate us on Spotify, apple podcasts or audible or whichever channel you are listening on. Challenges in supporting people with Personality Disorder is a common knowledge and skills deficits. Given severe borderline personality disorder has a standardised mortality rate of 45.1 it is a critical area for suicide prevention. Helping healthcare professionals fine tune their practice in this area is an essential step in creating a workforce that delivers high quality care for people in suicidal distress. Remember together we can make a difference. Tune in next Friday and we will explore how the AWARE factors relate to Borderline Personality Disorder. Thank you for joining us today and keep spreading the word.

